Disclaimer:
This page is not intent for commercial use; all information on this individual page (frame) is direct extraction from academic works to describe the pathology of individual prognosis. The intention of this page is to raise awareness to the general public for the implicated scientific findings and academic research purpose only.
免責聲明:
本頁面的資料由第三方學術研究抽取、參考;本頁面設立目的是為向公眾提倡有關病理科學知識及學術研究,並不打算用於商業用途。
1. 發病原因
1. 暗瘡
根据下列科學研究,暗瘡發病可歸咎於革蘭氏陽性菌,尤其是球菌類-
- 據A.D.A.M.醫學百科全書引述 -“...暗瘡是因皮膚面上的微小孔堵塞, 而這些孔被稱為毛孔... 當毛腺產生過多的油脂,可做成毛孔阻塞而令污垢、細菌積聚...”。[1]
- 日本京都大學一項研究發現 – “… 在19個沒有受暗瘡感染的人當中發現10個人的面上皮膚存有球菌… 在6個受到非炎性暗瘡感染的人當中發現5個的面上皮膚存有球菌。在炎性暗瘡個案中的毛孔及週邊毛孔發現存有球菌。”[2]
- 上述能肯定暗瘡發病徵兆大多數是因革蘭氏陽性細菌導至。
2. 特應性皮炎(過敏性濕疹)
特應性皮炎(過敏性濕疹)有許多發病原因;根據 “美國過敏、哮喘和免疫學院”和”歐盟過敏和臨床免疫學學院” 行的一份報告指出,該病發病模式如下:
圖1:從嬰兒期到成年導致特應性皮炎(過敏性濕疹)的多數原因[3]
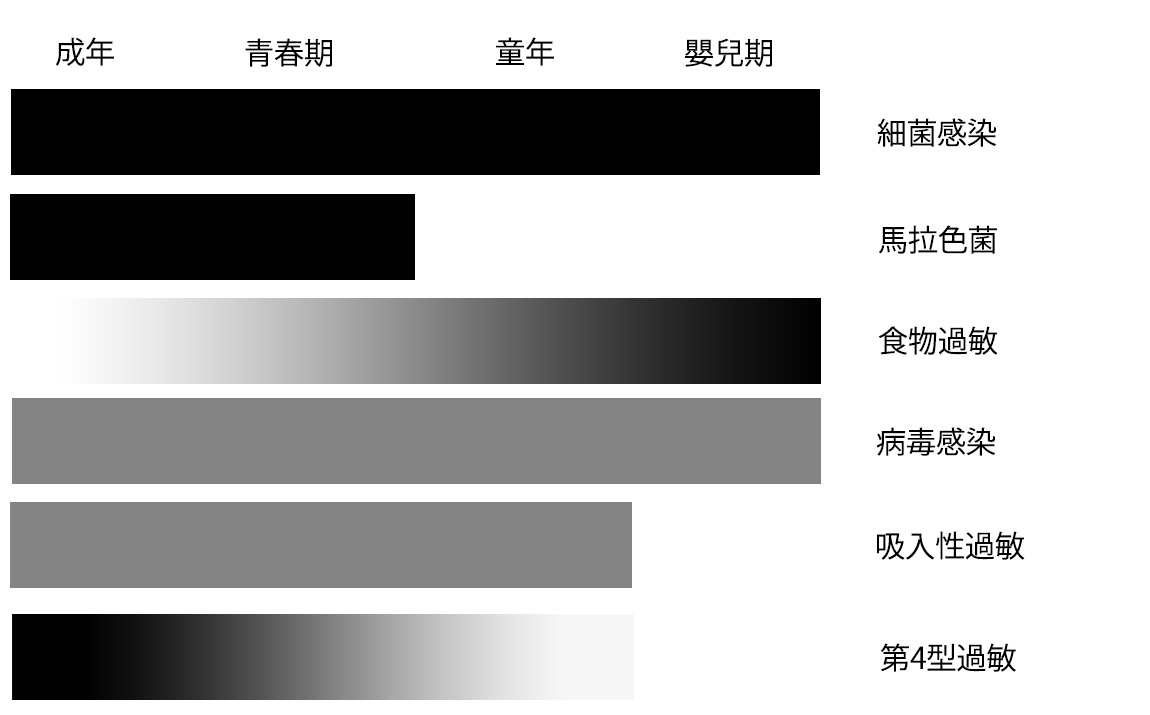
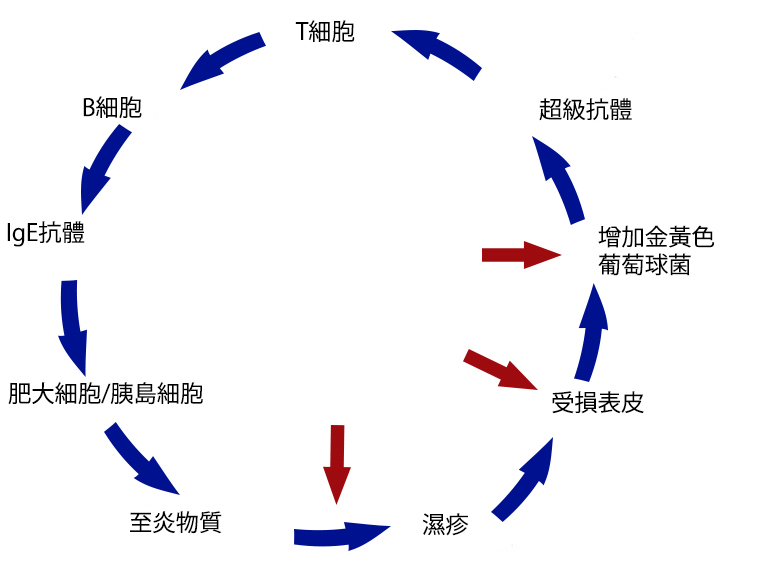
一項由Dr. Donald Y. M. Leung教授 (美國猶太醫學中心兒科、過敏和免疫專科主管,獲選為美國2012年頂尖醫生)發現,特應性皮炎(過敏性濕疹)的最主要微生物的因素是抗藥性金黃色葡萄球菌(MRSA),“超級細菌”。據文獻記載,“抗藥性金黃色葡萄球菌只會在55%-75%的非感染皮膚發現,並會在85%-91%的慢性苔蘚病形皮膚發現(痕痒而抓鬆了表皮),更會在80%-100%的急性滲出性皮膚病變發現(突發性的過敏性濕疹)。”[4] 研究還說明了孵化過敏性濕疹的發病週期,通俗地說 – “越痕痒便越抓,越抓便越痕痒(因更多細菌感染)”。
圖2:金黃色葡萄球菌在特應性皮炎(濕疹)的惡性循環。箭頭表示可以被打斷的惡性循環的地方。
[1] Berman, K., 2011, Acne: A.D.A.M. Medical Encyclopedia. U.S. National Library of Medicine. [Website] Available at:<http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001876/>[Accessed 19-01-2013]
[2]Imamura, S., 1972, The Localization and Distribution of Gram-Positive Cocci in Normal Skin and Lesions of Acne Vulgaris. Journal of Investigative Dermatology. [PDF] Available at: <http://www.nature.com/jid/journal/v65/n2/abs/5617211a.html>[Accessed 19-01-2013]
[3] Akdis, C.A., Akdis, M., Beiber, T., Boguniewicz, M., Eigenmann, P., Hamid, Q., Kapp, A., Leung, D.Y.M., Lipozencic, J., Luger, T.A., Muraro, A., Novak, N., Platt-Mills, T.A.E., Rosenwasser, L., Scheynius, A., Simons, F.E.R., Spergel, J., Turjanmaa, K., Wahn, U., Weidinger, W., Werfel, T., Zuberbier, T., 2006. Diagnosis and treatment of atopic dermatitis in children and adults: European Academy of Allergology and Clinical Immunology/American Academy of Allergy, Asthma and Immunology/PRACTALL Consensus Report. American Academy of Allergy, Asthma and Immunology and the European Academy of Allergology and Clinical Immunology. [PDF] Available at: <http://onlinelibrary.wiley.com/doi/10.1111/j.1398-9995.2006.01153.x/pdf> [Accessed 24-12-2012]
[4], [5] Leung, Y.M. D., 2008. 3. The role of Staphylococcus aureus in atopic eczema. Acta Derm Venereol. [PDF] Available at: <https://www.google.com.hk/url?sa=t&rct=j&q=&esrc=s&source=web&cd=1&ved=0CDkQFjAA&url=http%3A%2F%2Fwww.medicaljournals.se%2Facta%2F content%2Fdownload.php%3Fdoi%3D10.2340%2F00015555-0388&ei=A2vaUKzoMemTiAeYvoHQAw&usg=AFQjCNECZudbTcsvUEylo3MtFJzBiNdlGg&bvm=bv.1355534169,d.aGc&cad=rja> [Accessed 26-12-2012]









Follow us